Menu
•
Background luminance might sound like a technical specification buried in device manuals, but for ophthalmologists and optometrists, it’s a crucial factor in visual field testing. In Standard Automated Perimetry (SAP), background luminance refers to the constant light level presented on the bowl or screen in areas where the stimulus (e.g., Goldmann III) is not presented. This seemingly simple parameter plays a major role in the accuracy and reliability of visual field test results.¹ It’s also a key parameter that distinguishes the Topcon Inspire® headset powered by RadiusXR® from competing devices. Unlike many competitors, Inspire adheres to clinical standards for background luminance. In this article, we will examine the clinical standard for SAP background luminance and why it matters for disease management.
In SAP – the common “white-on-white” visual field test used in clinics – a patient looks into a uniformly illuminated bowl or screen while a small spot of light (e.g., Goldmann III) is presented at different test locations. The Humphrey Field Analyzer (HFA), the current clinical standard in SAP, uses a uniform background luminance of 10 cd/m² (approximately 31.5 apostilbs).¹ The choice of 10 cd/m² is not arbitrary. It is near the lower boundary of photopic (daylight) vision where the only photoreceptors active are cones (no rods are active at 10 cd/m²).² In practice, this means that the background is a dim white glow, not completely dark, not very bright, but equivalent to about 10 candles spread over a square meter. The Inspire headset’s visual field test replicates this precisely, presenting targets on a 10 cd/m² background, intentionally matching the HFA’s conditions.

Background luminance has critical implications for test accuracy and clinical relevance:
A background luminance of 10 cd/m² ensures that visual field sensitivity is estimated in photopic viewing conditions. This matters because many virtual reality perimeters (VRP) perform visual field testing in mesopic (0.01–3 cd/m²) conditions where both rods and cones are active, or even in scotopic (< 0.01 cd/m²) conditions where only rods are active.² It is well known that sensitivities estimated under mesopic or scotopic conditions are poorly correlated with sensitivities estimated under photopic conditions.³,⁴ In other words, when the background is too dim, rods become active, altering the sensitivity and making results less comparable to clinical standards for automated perimetry.
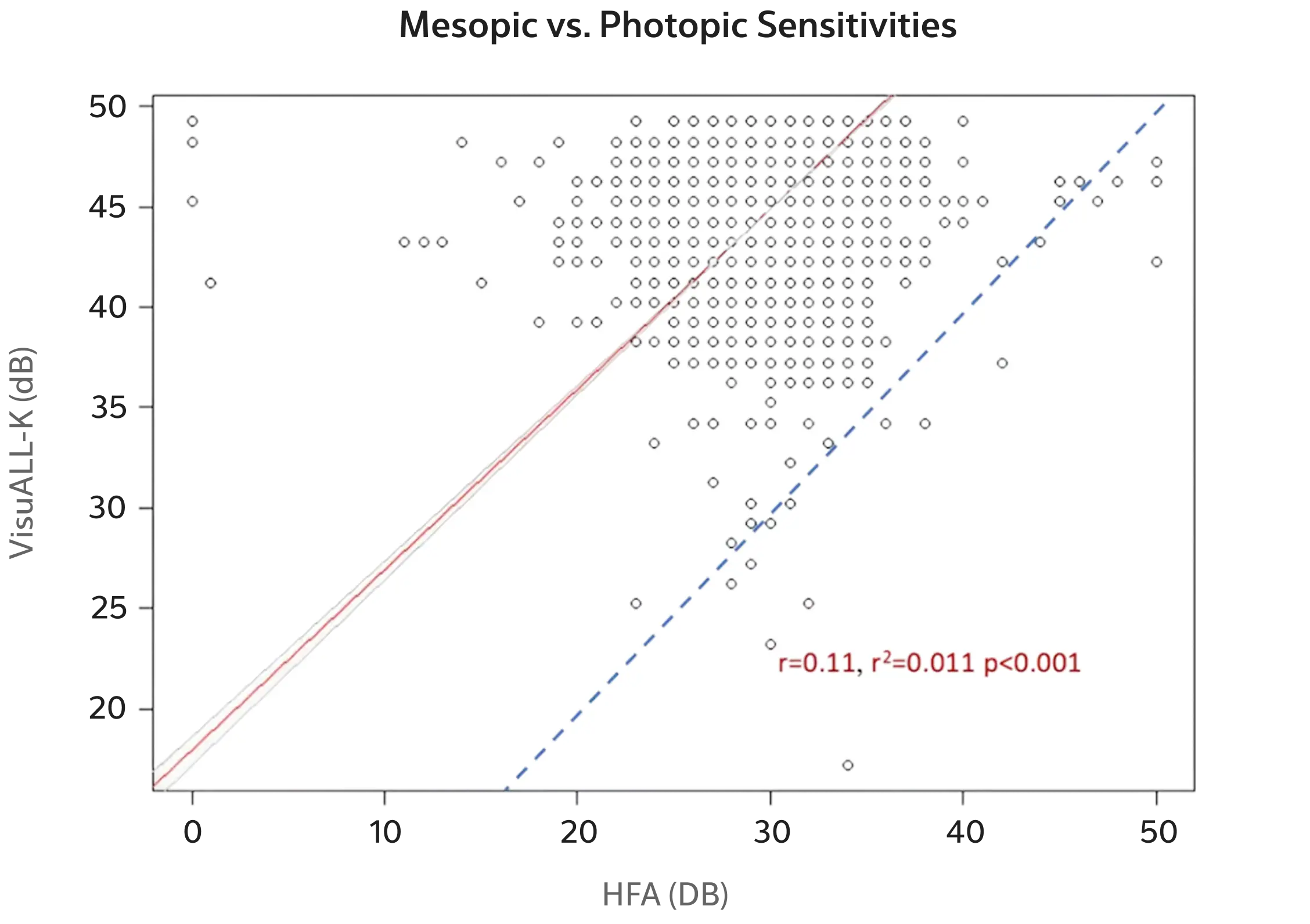
Figure 1.
Comparison of pointwise sensitivities from the VisuALL-K algorithm of the Olleyes VRP to pointwise sensitivities estimated by the clinical standard HFA.
Today’s innovations in perimetry often focus on portability and efficiency such as lightweight headsets that can perform visual field testing in a clinic hallway or in a patient’s home. However, not all such devices are equal in faithfully reproducing clinical-standard test conditions. Many VRPs test in the mesopic range where both cones and rods are active. For example, Figure 1 shows an example of pointwise sensitivities for the Olleyes VRP using their VisuALL-K algorithm compared to the HFA. The correlation is very low (r = 0.11), and most sensitivity estimates with the VisuALL-K are well above the identity line (dotted line) — sensitivities are systematically higher when testing on a darker, mesopic background luminance.⁵–⁷
In contrast, the Inspire headset powered by Radius XR uses the same background luminance as the HFA. A recent study showed no statistically significant differences in pointwise sensitivities between the RATA-Standard algorithm of the Inspire and the SITA-Standard algorithm of the HFA within the 15–40 dB measurement range of the Inspire.⁸ The Inspire sacrifices measurement range — a result of performing VRP in a headset with less power than a tabletop device like the HFA — for high concordance in estimated sensitivities. The result is that the Inspire by RadiusXR can replace or complement traditional perimeters without compromising on test quality. You get the same photopic testing environment, but delivered through a lightweight, patient-friendly device that doesn’t require a dark room or a bulky bowl apparatus.
For eye care practitioners evaluating new visual field testing options, understanding background luminance is important. A device that cuts corners on this parameter might produce visual fields that correlate poorly with familiar Humphrey results. Small deviations in test conditions can lead to misleading outcomes. For instance, a lower background luminance could artificially inflate sensitivity, potentially underestimating the degree of field loss or changing the appearance of defects.³,⁴
Another implication is patient experience and clinic workflow. Because the headset has a light seal that prevents ambient light from entering, it is not necessary to test in a dark room with a special setup. Patients can take the test in various settings, even a waiting room. This allows more flexibility in when and where tests are done, potentially increasing throughput without sacrificing quality.⁸
Background luminance is a key visual field test parameter. Testing on a standardized 10 cd/m² background luminance is essential to ensure sensitivities are comparable to the HFA. The good news is that innovations like the Inspire headset by RadiusXR have fully recognized the importance of background luminance. By supporting the standard background luminance and other key parameters, we have made it possible to bring visual field testing into new settings – portable, patient-guided testing – without compromising on clinical accuracy.
RadiusXR is transforming vision testing and eye care with an advanced digital platform that enables unrivaled patient access, streamlines operations, and creates more confidence at the point of care. Our clinically validated portable platform integrates seamlessly into existing systems, with customized software and cloud technology to securely manage data and a lightweight, purpose-built headset. With our advanced wearable technologies, we continue developing disruptive technologies that challenge the healthcare status quo.
Mon – Fri 5:00 am – 5:00 pm PST